WHICH DIALYSIS ACCESS CARE TREATMENTS ARE AVAILABLE FOR A DYSFUNCTIONAL ACCESS?
When an Arteriovenous Fistula (called an AVF) or Arteriovenous Graft (called an AVG) clots or narrows, blood flow through the access is decreased, which impacts your ability to undergo a scheduled dialysis treatment. If your access does not work properly, your nephrologist may prescribe an interventional procedure to improve the blood flow through your access. There are several minimally invasive procedures available that can treat a dysfunctional access, allowing you to return to your regularly scheduled dialysis treatments quickly.
FISTULAGRAM
A fistulagram is a procedure that employs use of a live X-Ray. After inserting a small catheter into the fistula, contrast dye is injected under live X-Ray. This allows Dr. Kahn to view the blood flow and check for narrowings or blockages in the fistula or graft. When narrowings or blockages are identified, they are fixed using a balloon and occasionally a stent when additional support is needed.
During this procedure, you will lie on a bed with your arm extended to the side. Our nurse will connect you to a monitor to assess your heart rate, blood pressure, and oxygenation during the procedure. A small IV is placed in the opposite arm to allow sedative drugs to be administered throughout the procedure. You will be covered with a sterile drape, with the fistula or graft left exposed for access. A local anesthetic is administered at the planned site(s) of access. Dr. Kahn inserts one or two small catheters into the fistula or graft at the beginning of the procedure. Contrast dye or carbon dioxide (CO2) gas is injected, which allows blood flow within the fistula or graft to be visualized under X-Ray. Areas that are problematic are then readily identified by Dr. Kahn.
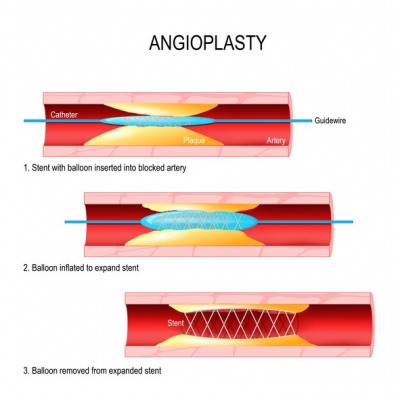
ANGIOPLASTY AND STENTING OF THE FISTULA
Angioplasty is a minimally invasive solution to fix a vessel that is narrowed or blocked. A wire is threated through the problematic area. The wire serves as a “rail” over which a special type of balloon is advanced to the site of the narrowing or blockage. The balloon is then inflated to a high pressure and used to re-open the fistula or graft to the desired diameter. You may feel some discomfort while the balloon is inflated, but this is minimized by the sedation. After the balloon is deflated and removed, contrast dye or CO2 is re-injected under live X-Ray to evaluate improvement of the blood flow.
On occasion, the balloon alone does not provide an adequate result because the fistula or graft immediately re-narrows after balloon angioplasty. In these situations, a stent may be necessary. A stent is a small metallic tube-shaped scaffolding that is commonly lined with a fabric-like material. It is designed to hold a vessel, fistula, or graft open after deployment. The stent is a permanent implant that remains in place.
Once the procedure is complete, you will be taken to our recovery area. You will be observed prior to being discharged. There may be some discomfort after the procedure that can be treated with over-the-counter medication. Heavy lifting or strenuous exercise is discouraged after the procedure.
PLACEMENT OF TUNNELED CENTRAL CATHETERS FOR DIALYSIS
Dialysis catheters are dual lumen catheters that are inserted through the skin into a vein with the tip located in or near the heart. These catheters are considered a temporary dialysis option for patients that do not have a more permanent option, such as a peritoneal dialysis catheter, a fistula, or a graft. The catheters allow rapid removal of blood to the dialysis machine through one of the two lumens and rapid return of the blood to the patient from the machine through the other lumen. Dialysis catheters can be placed temporarily directly into the vein, but these catheters are typically only used on a very short-term basis, such as during a hospitalization. More commonly these catheters are tunneled under the skin for a short distance before entering the vein. Tunneling a catheter under the skin provides greater patient comfort, prevents infection, and secures the catheter for longer term use. The catheters can be placed in a variety of locations, including the neck, chest, legs, and trunk, but the neck and chest are the most common sites.
During the procedure, a catheter placement will typically take less than a half hour. You will lie flat on the procedure table with your neck and chest prepared in a sterile manner. Surgical drapes are placed around the access site. If desired, you can receive a sedative through an IV line placed in the hand or arm. Dr. Kahn uses an ultrasound machine to locate the vein that will be used and anesthetizes the overlying skin with a local anesthetic. Dr. Kahn then makes a small incision at the base of the neck or chest before inserting a needle under ultrasound guidance into the vein. Once in the vein, a wire is threaded into the vein through the needle and the needle is subsequently removed.
Additional local anesthetic is administered along the planned tract of the catheter under the skin and a separate small incision is made at the anticipated catheter exit site. The catheter is then threaded under the skin from the exit site to the vein access site. Through a special type of sheath, the catheter is then
threaded into the vein and live X-Ray guidance is used to confirm the catheter position. The catheter is tested and then secured with a stitch to the skin. The catheter will be ready for immediate use.
During the recovery, you will be moved to a recovery room to be monitored by our nurse. Typically, the recovery period is brief and patients can be discharged home shortly after the procedure. It is normal for you to experience some discomfort after the procedure that is typically relieved by over-the-counter medication. Swelling or bruising at the site of the catheter may occur. Strenuous activity or heavy lifting is discouraged for several days after the procedure.
PLACEMENT OF TUNNELED CENTRAL CATHETERS FOR DIALYSIS
Peritoneal dialysis is an alternative to hemodialysis and is preferable to some patients, as it can be done easily at home. A peritoneal dialysis catheter is placed in the abdomen, below or to the left or right of the navel. This procedure typically takes less than an hour, and you will likely be able to leave shortly thereafter. Your abdomen and pelvis will be inspected before the procedure. Measurements for the planned catheter placement are obtained and marked on your skin.
Prior to the procedure, you will be transferred to the procedure room where you will lie flat on the exam table. Sedative drugs are administered, your abdomen is then sterilized, and a local anesthetic is administered at the planned catheter placement site.
After administering the local anesthetic, a small incision is made in the abdomen. Ultrasound and live X-Ray guidance are then used to advance a small needle into the abdominal cavity. Contrast dye is injected through the needle under live X-Ray to confirm the needle is properly located in the abdominal cavity. After confirming needle position, roughly a half liter of saline is infused into the abdominal cavity to facilitate easy placement of the catheter.
A wire is then guided through the needle into the abdomen. Once the wire is in place, the needle is removed. A dilator and peel-away-sheath are inserted over the guidewire into the abdominal cavity. When the sheath is in place, the dilator and wire are removed and the catheter is placed through the sheath. The sheath is removed and live X-Ray is used to confirm that the catheter tip is in the lower pelvis. The catheter position is important to optimize fluid administration and drainage from the most dependent portion of the abdominal cavity. The catheter is tested with the injection of saline and contrast dye to confirm its function and position. Once confirmed, the other end of the catheter is then threaded under the skin to a separate small incision made in the skin at the catheter exit site. The original small incision is stitched closed and the catheter is secured with a sterile dressing at its exit site.
During the recovery, you will be moved to the recovery area and monitored. You may experience minor discomfort that is usually managed with over-the-counter medications. Heavy lifting or strenuous activities are discouraged after the procedure. Care of the catheter is particularly important to prevent infection. Use of the catheter is discouraged for at least a couple of weeks after placement. Additionally, patients are instructed to follow up with the dialysis center within one week of catheter placement for testing and dressing changes.
THROMBECTOMY-THROMBOLYSIS PROCEDURE
Blood clots that develop in a dialysis access need to be treated to restore blood flow through the access. A combination of instruments and clot dissolving drugs are used to remove the clot and restore blood flow. Clot dissolving drugs are delivered directly to the clot and allowed to saturate the clot thereby dissolving it.
In addition, balloons and several mechanical devices are available to further break-up and remove the blood clot from the fistula or graft. As with all fistulagram procedures, you will be given a local anesthetic to numb the area and a moderate sedative is given to help you relax.
MILLER BANDING PROCEDURE FOR STEAL SYNDROME
Steal Syndrome may develop in some patients who have a fistula or graft. This syndrome is characterized by insufficient blood flow to the hand caused by excessive diversion of blood flow to the fistula or graft. The hand thereby receives inadequate blood flow. Symptoms of steal syndrome include pain, coldness, numbness, or tingling in the hand and patients may notice a pale hand color. In severe cases, wounds or tissue loss can occur in the fingers and hands. if you experience any of these symptoms, it is important to speak to your physician immediately. There are minimally invasive procedures that can be used to treat steal syndrome.
Minimally Invasive Limited Ligation Endoluminal-assisted Revision (AKA The Miller Procedure) is used to balance blood flow through a dialysis access so that there is adequate circulation to the hand. The access is adjusted to the proper size by using an angioplasty balloon as a sizing dowel and banding the access to the measured size. During the recovery, you may be prescribed some pain medication to help with any discomfort, but you should be able to return to daily activities within 24 hours.
What are the Benefits of Minimally Invasive Treatments of a Dysfunctional Access?
Treating a dysfunctional access with minimally invasive procedures to correct blood flow offers several benefits:
- Avoids the need for general anesthesia and the associated risks
- Quick return to daily activities
- Resume or continue your scheduled dialysis treatments without interruption
- Decreased procedural risks, including infection
- Safely performed as an outpatient, without the need for hospitalization
We Can Help!
New England Endovascular Center offers expertise, state-of-the-art imaging, and resources for dialysis access management. We customize each patient’s treatment plan to maximize the best possible outcome. We are committed to providing excellent, personal patient care.
Call our office today to schedule a consultation at 413-693-2852.

Our providers are nationally recognized experts in minimally invasive therapies for treating dialysis access care and maintenance.
We provide fistula maintenance to patients throughout Western MA and Northern CT.
To learn more about treatments available at New England Endovascular Center call 413-693-2852 to make an appointment.
